Giving to your state PAC is one the BEST ways to support your profession.
BE PART OF THE SOLUTION AND NOT PART OF THE POLLUTION and STOP the AMA & ASA from actively campaigning against your ability to practice to your full scope, education, and licensure.
Delegates voice concerns regarding dangers of anesthesia bill which passes through House
February 1, 2023
"Delegate Summers addressed her fellow Delegates at the close of debate on the bill stating,
“I’ll just say one thing, in my 37 years of experience as a nurse, I could tell you all kinds of stories to support whatever position I want to support. But that’s not what this bill is about. All this bill is about is making our laws be in alignment with what the CNA’s are trained to do. I’m just asking that we push green to align their scope with our laws.”
"House Bill 2613 was ultimately communicated to the Senate upon passage through the House with 77 yeas, 21 nays, and 2 voting Delegates counted as absent from the proceedings."
Many Anesthesiologists Do Not Accurately Report Anesthesia Start Time
January 30, 2023
"Most operating room (OR) cases do not properly document the anesthesia start time (AST), resulting in thousands of dollars in lost revenue for hospitals, according to a study presented at the American Society of Anesthesiologists ADVANCE 2023, Anesthesiology Business Event, held from Jan. 27 to 29 in Orlando, Florida."
"The researchers found that of all OR cases occurring between Nov. 1, 2021, and Oct. 31, 2022, 68.74 percent had AST documented after the IRT. Using the corrected AST value, this translated to 136,858.19 minutes of lost anesthesia time and 9,123.88 lost ATUs, corresponding to $638,671.57 of lost revenue for the hospital."
Long COVID patients turn to experimental treatment to fix altered sense of smell - CRNAs have the answer
January 26, 2023
BRYAN, Texas — Within the walls of this unassuming office, thousands of people are turning to the medical professionals here for hope.
"We're a pain practice, so we treat chronic pain,” said David Gaskin, a certified registered nurse anesthetist with Republic Pain Specialists in Bryan, Texas.
If WA state lawmakers mess with anesthesia care, they’ll be doing more harm than good
January 23, 2023
"One idea that doesn’t make sense is a controversial proposal to allow for something in our state called an anesthesiologist assistant (AA). Adding yet another type of job to fit through the same clogged pipeline for training health care professionals will make it even harder for our existing care providers to get trained, making the staffing crisis worse. AAs are not allowed to provide anesthesia care to patients without a physician present. This means more physician anesthesiologists will be needed to help the same amount of people, and our staffing shortage will be left unaddressed."
Wearable Sensor Uses Ultrasound to Provide Cardiac Imaging On the Go
January 25, 2023
"Engineers and physicians have developed a wearable ultrasound device that can assess both the structure and function of the human heart. The portable device, which is roughly the size of a postage stamp, can be worn for up to 24 hours and works even during strenuous exercise."
"The goal is to make ultrasound more accessible to a larger population, said Sheng Xu, a professor of nanoengineering at the University of California San Diego, who is leading the project. Currently, echocardiograms– ultrasound examinations for the heart– require highly trained technicians and bulky devices."
“The technology enables anybody to use ultrasound imaging on the go,” Xu said."
I Am Navy Medicine – and Certified Registered Nurse Anesthetist – Lt. Jason Balazs
January 25, 2023
Naval Hospital Bremerton/Navy Medicine Readiness and Training Command Bremerton
"Whether it’s preoperative, intraoperative, or postoperative for any surgery or procedure in Naval Hospital Bremerton’s Main Operating Room, Lt. Jason Balazs is easy to locate.
As a certified registered nurse anesthetist, Balazs is constantly providing critical care services to every patient in need.
Such expertise and attention to detail by him, as well as other certified registered nurse anesthetists, is recognized with National CRNA Week, January 22-28, 2023. The annual event was initially established by the American Association of Nurse Anesthetists to acknowledge the anesthetist profession's long history and enduring record of patient safety.
CRNAs like Balazs provide critical care services such as reviewing a patient’s medical history and providing anesthesia to that patient before the surgery/procedure, monitoring the patient’s vitals during the surgery/procedure and afterwards overseeing the patient’s recovery from the anesthesia and help provide any additional post-operative care."
FGCU nurse anesthesiologists will be doctors for first time
January 25, 2023
"Florida Gulf Coast University has been training nurse anesthesiologists since about 2006, but it’s still not a well-known specialty.
Dr. Robert Bland teaches in the program.
“Nurse anesthesiology is basically the same as medical anesthesiology in that we provide perioperative care to any patients needing surgery or anesthesia for procedures,” he said.
This year is the first year that all graduates of this program will have a doctorate of nursing practice (or DNP)."
AS Virginia Faces Anesthesia Provider Shortage:
ANESTHESIA EXPERTS AT THE READY
Column: A simple change can improve health care
By Meredith Joyner
January 21, 2023
"Virginia is one of only a handful of states to continue having supervision language as a requirement for CRNAs, making it an outlier. By modernizing the language that governs the practice of CRNAs to allow for consultation, legislators would help hospitals and surgical facilities fully use all of the anesthesia experts available to them, resulting in care for more patients needing surgery."
Demand for anesthesia providers is growing as reimbursement is shrinking, says NorthStar Anesthesia CEO
January 19, 2023
""The problem is, during the pandemic, like every other workforce, we actually saw a contraction in the number of providers," Mr. Spiegel said. "People retired early, people decided that they could go part time, some just decided to leave the workforce altogether. And as a result, we've been in this situation where demand far exceeds supply when it comes to anesthesia providers."
"As the demand for anesthesiologists and CRNAs continues to climb, so do their salaries. Mr. Spiegel explained that anesthesia providers are only partially compensated by the revenue NorthStar earns from each case."
Jessie Bozelka: Proposed anesthesia staffing changes won’t help patients
January 15, 2023
"There is currently a staffing crisis in health care, and our elected leaders in Olympia are fielding several ideas on how to address this crisis so that more patients have better access to quality care. There are many types of medical professionals that staff hospitals, but I will focus on anesthesia care because that is what I know best. CRNAs like myself are board certified and licensed in our state to provide anesthesia care for patients independent of physician supervision. This means we are able to offer quality anesthesia care in places where there are not physician anesthesiologists – in fact, CRNAs work in 93% of all rural hospitals in Washington and are the only provider of anesthesia in 72% of these hospitals in smaller communities. We are also the primary provider of anesthesia for those serving in our nation’s military. CRNAs are qualified to provide care independently due to strict requirements for our education and clinical training – we have an average of four and half years of clinical experience in ICUs before starting our doctorate degree, more than 12,000 hours of clinical care experience by the time we graduate and study from the same textbooks and courses that are required for physician anesthesiologists during their education. The current staffing crisis means that more than ever, I am proud that I have the ability to serve patients independently if needed and assist in increasing access to care."
Nurse anesthetists could ease staffing shortages, but most Montana physicians say no thanks
January 14, 2023
"Certified Registered Nurse Anesthetists (CRNA) are qualified to administer every type of anesthesia, and they provide 100% of the anesthesia services in rural Montana, Carter said. And they do so without the supervision of a physician anesthesiologist."
"As the physician shortage has worsened over the years, exacerbated by burnout from the COVID pandemic, CRNAs have advertised themselves as a viable solution to staffing challenges in the state’s metropolitan areas.
The shortage of anesthesiologists isn’t a new issue. Staffing researchers warned of developing shortfalls about 20 years ago when the need for services began stretching into nearly every department in the hospital, according to Dr. Randall Clark, president of the American Society of Anesthesiology. Since then, anesthesiology departments have struggled to keep up with the rapidly changing health care landscape and demand has since far outpaced supply."
Nurse Anesthesia Doctoral Candidates Receive Traditional White Coats
January 14, 2023
"Southern Illinois University Edwardsville School of Nursing (SON) recognized 32 nurse anesthesia doctoral candidates during a traditional White Coat Ceremony held Tuesday, Jan. 10. The traditional ceremony symbolizes the transition into the clinical portion of the nurse anesthesia Doctor of Nursing Practice (DNP) specialization."
“The White Coat Ceremony is a rite of passage symbolizing how hard these students have worked over the past year in the program and how far they have come in such a short time,” said Kevin Stein, DNAP, CRNA, chair of the SON’s Department of Nurse Anesthesiology. “The relationships these students have built with one another will serve as much-needed support network as they continue to navigate the rigors of the program.”
FTC Considers: Non-Compete Clause Rulemaking
January 13, 2022
"About one in five American workers—approximately 30 million people—are bound by a non-compete clause and are thus restricted from pursuing better employment opportunities. A non-compete clause is a contractual term between an employer and a worker that blocks the worker from working for a competing employer, or starting a competing business, typically within a certain geographic area and period of time after the worker’s employment ends. Because non-compete clauses prevent workers from leaving jobs and decrease competition for workers, they lower wages for both workers who are subject to them as well as workers who are not. Non-compete clauses also prevent new businesses from forming, stifling entrepreneurship, and prevent novel innovation which would otherwise occur when workers are able to broadly share their ideas."
"The Federal Trade Commission proposes preventing employers from entering into non-compete clauses with workers and requiring employers to rescind existing non-compete clauses. The Commission estimates that the proposed rule would increase American workers’ earnings between $250 billion and $296 billion per year. The Commission is asking for the public’s opinion on its proposal to declare that non-compete clauses are an unfair method of competition, and on the possible alternatives to this rule that the Commission has proposed."
Opioid-free anesthesia: the next frontier in surgical patient safety
December 2, 2022
"The intuitive next frontier for streamlining our patients’ perioperative care and improving surgical patient safety and patient outcomes is represented by the proactive (and arguably provocative) concept of opioid-free anesthesia. The primary goal of opioid-free anesthesia is to abstain from the use of mu receptor agonists through the use of non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen, lidocaine, dexmedetomidine, ketamine, and low-dose glucocorticoids. In addition, regional nerve blocks represent a fundamental pillar of intra- and postoperative analgesia as part of the opioid-free anesthesia protocol."
Kate Jansky and Randall Moore eloquently dropped truth bombs 💣 on ASA fibs, many which are still repeated ad-nauseum today
November 9, 2022
𝘞𝘩𝘦𝘯 𝘸𝘦 𝘸𝘦𝘳𝘦 𝘤𝘩𝘪𝘭𝘥𝘳𝘦𝘯, 𝘰𝘶𝘳 𝘱𝘢𝘳𝘦𝘯𝘵𝘴 𝘵𝘢𝘶𝘨𝘩𝘵 𝘶𝘴 𝘵𝘰 𝘢𝘭𝘸𝘢𝘺𝘴 𝘵𝘦𝘭𝘭 𝘵𝘩𝘦 𝘵𝘳𝘶𝘵𝘩. 𝘐𝘯 𝘵𝘩𝘦 𝘮𝘪𝘭𝘪𝘵𝘢𝘳𝘺, 𝘸𝘦 𝘸𝘦𝘳𝘦 𝘵𝘢𝘶𝘨𝘩𝘵 𝘵𝘰 𝘷𝘢𝘭𝘶𝘦 𝘪𝘯𝘵𝘦𝘨𝘳𝘪𝘵𝘺. 𝘈𝘴 𝘊𝘦𝘳𝘵𝘪𝘧𝘪𝘦𝘥 𝘙𝘦𝘨𝘪𝘴𝘵𝘦𝘳𝘦𝘥 𝘕𝘶𝘳𝘴𝘦 𝘈𝘯𝘦𝘴𝘵𝘩𝘦𝘵𝘪𝘴𝘵𝘴 (𝘊𝘙𝘕𝘈𝘴), 𝘸𝘦 𝘭𝘦𝘢𝘳𝘯𝘦𝘥 𝘵𝘩𝘦 𝘯𝘦𝘤𝘦𝘴𝘴𝘪𝘵𝘺 𝘰𝘧 𝘴𝘤𝘪𝘦𝘯𝘤𝘦 𝘢𝘯𝘥 𝘦𝘷𝘪𝘥𝘦𝘯𝘤𝘦. 𝘈𝘴 𝘱𝘢𝘳𝘦𝘯𝘵𝘴, 𝘸𝘦 𝘩𝘢𝘷𝘦 𝘭𝘦𝘢𝘳𝘯𝘦𝘥 𝘵𝘩𝘢𝘵 “𝘣𝘦𝘤𝘢𝘶𝘴𝘦 𝘐 𝘴𝘢𝘺 𝘴𝘰” 𝘪𝘴 𝘯𝘰𝘵 𝘢𝘯 𝘢𝘳𝘨𝘶𝘮𝘦𝘯𝘵 𝘵𝘩𝘢𝘵 𝘤𝘢𝘳𝘳𝘪𝘦𝘴 𝘢𝘯𝘺 𝘸𝘦𝘪𝘨𝘩𝘵. 𝘠𝘦𝘵, 𝘵𝘩𝘢𝘵 𝘪𝘴 𝘱𝘳𝘦𝘤𝘪𝘴𝘦𝘭𝘺 𝘸𝘩𝘢𝘵 𝘵𝘩𝘦 𝘈𝘮𝘦𝘳𝘪𝘤𝘢𝘯 𝘚𝘰𝘤𝘪𝘦𝘵𝘺 𝘰𝘧 𝘈𝘯𝘦𝘴𝘵𝘩𝘦𝘴𝘪𝘰𝘭𝘰𝘨𝘪𝘴𝘵𝘴 (𝘈𝘚𝘈) 𝘤𝘰𝘯𝘴𝘪𝘴𝘵𝘦𝘯𝘵𝘭𝘺 𝘳𝘦𝘭𝘪𝘦𝘴 𝘰𝘯 𝘵𝘰 𝘴𝘤𝘢𝘳𝘦 𝘵𝘩𝘦 𝘱𝘶𝘣𝘭𝘪𝘤 𝘪𝘯𝘵𝘰 𝘣𝘦𝘭𝘪𝘦𝘷𝘪𝘯𝘨 𝘵𝘩𝘢𝘵 𝘊𝘙𝘕𝘈𝘴 𝘢𝘳𝘦 𝘯𝘰𝘵 𝘴𝘢𝘧𝘦. 𝘜𝘯𝘧𝘰𝘳𝘵𝘶𝘯𝘢𝘵𝘦𝘭𝘺 𝘧𝘰𝘳 𝘵𝘩𝘦𝘮, 𝘵𝘩𝘪𝘴 𝘫𝘶𝘴𝘵𝘪𝘧𝘪𝘤𝘢𝘵𝘪𝘰𝘯 𝘥𝘰𝘦𝘴𝘯’𝘵 𝘸𝘰𝘳𝘬 𝘸𝘪𝘵𝘩 𝘤𝘩𝘪𝘭𝘥𝘳𝘦𝘯 𝘢𝘯𝘥 𝘤𝘦𝘳𝘵𝘢𝘪𝘯𝘭𝘺 𝘩𝘢𝘴 𝘯𝘰 𝘱𝘭𝘢𝘤𝘦 𝘪𝘯 𝘱𝘰𝘭𝘪𝘤𝘺𝘮𝘢𝘬𝘪𝘯𝘨. 𝘠𝘦𝘵, 𝘵𝘩𝘪𝘴 𝘦𝘷𝘪𝘥𝘦𝘯𝘤𝘦-𝘧𝘳𝘦𝘦 𝘢𝘳𝘨𝘶𝘮𝘦𝘯𝘵 𝘪𝘴 𝘢𝘭𝘭 𝘵𝘩𝘦𝘺 𝘩𝘢𝘷𝘦, 𝘴𝘪𝘯𝘤𝘦 𝘢𝘭𝘭 𝘤𝘳𝘦𝘥𝘪𝘣𝘭𝘦 𝘦𝘷𝘪𝘥𝘦𝘯𝘤𝘦 𝘴𝘩𝘰𝘸𝘴 𝘵𝘩𝘢𝘵 𝘊𝘙𝘕𝘈𝘴 𝘱𝘳𝘰𝘷𝘪𝘥𝘦 𝘵𝘩𝘦 𝘩𝘪𝘨𝘩𝘦𝘴𝘵 𝘲𝘶𝘢𝘭𝘪𝘵𝘺 𝘤𝘢𝘳𝘦 𝘳𝘦𝘨𝘢𝘳𝘥𝘭𝘦𝘴𝘴 𝘰𝘧 𝘱𝘳𝘢𝘤𝘵𝘪𝘤𝘦 𝘴𝘦𝘵𝘵𝘪𝘯𝘨 𝘰𝘳 𝘱𝘢𝘵𝘪𝘦𝘯𝘵𝘴’ 𝘩𝘦𝘢𝘭𝘵𝘩 𝘴𝘵𝘢𝘵𝘶𝘴. 𝘐𝘵’𝘴 𝘸𝘩𝘺 𝘊𝘙𝘕𝘈𝘴 𝘢𝘳𝘦 𝘵𝘩𝘦 𝘴𝘰𝘭𝘦 𝘢𝘯𝘦𝘴𝘵𝘩𝘦𝘴𝘪𝘢 𝘱𝘳𝘰𝘷𝘪𝘥𝘦𝘳𝘴 𝘰𝘯 𝘧𝘰𝘳𝘸𝘢𝘳𝘥 𝘴𝘶𝘳𝘨𝘪𝘤𝘢𝘭 𝘵𝘦𝘢𝘮𝘴 𝘢𝘯𝘥 𝘵𝘩𝘦 𝘱𝘳𝘦𝘥𝘰𝘮𝘪𝘯𝘢𝘯𝘵 𝘢𝘯𝘦𝘴𝘵𝘩𝘦𝘴𝘪𝘢 𝘱𝘳𝘰𝘷𝘪𝘥𝘦𝘳𝘴 𝘪𝘯 𝘳𝘶𝘳𝘢𝘭 𝘢𝘳𝘦𝘢𝘴. 𝘐𝘵 𝘪𝘴 𝘸𝘩𝘺 𝘊𝘙𝘕𝘈𝘴 𝘢𝘳𝘦 𝘴𝘵𝘦𝘱𝘱𝘪𝘯𝘨 𝘶𝘱 𝘰𝘯 𝘵𝘩𝘦 𝘧𝘳𝘰𝘯𝘵 𝘭𝘪𝘯𝘦𝘴 𝘥𝘶𝘳𝘪𝘯𝘨 𝘵𝘩𝘦 𝘤𝘶𝘳𝘳𝘦𝘯𝘵 𝘊𝘖𝘝𝘐𝘋-19 𝘤𝘳𝘪𝘴𝘪𝘴, 𝘢𝘴 𝘴𝘦𝘳𝘪𝘰𝘶𝘴 𝘱𝘰𝘭𝘪𝘤𝘺𝘮𝘢𝘬𝘦𝘳𝘴 𝘴𝘦𝘦𝘬 𝘵𝘰 𝘳𝘦𝘮𝘰𝘷𝘦 𝘣𝘢𝘳𝘳𝘪𝘦𝘳𝘴 𝘵𝘰 𝘰𝘶𝘳 𝘱𝘳𝘢𝘤𝘵𝘪𝘤𝘦 𝘢𝘵 𝘵𝘩𝘦 𝘴𝘵𝘢𝘵𝘦 𝘢𝘯𝘥 𝘯𝘢𝘵𝘪𝘰𝘯𝘢𝘭 𝘭𝘦𝘷𝘦𝘭𝘴.
𝘙𝘦𝘤𝘦𝘯𝘵𝘭𝘺 𝘵𝘩𝘦 𝘈𝘚𝘈 𝘱𝘶𝘵 𝘰𝘶𝘵 𝘢 𝘩𝘪𝘨𝘩𝘭𝘺 𝘮𝘪𝘴𝘭𝘦𝘢𝘥𝘪𝘯𝘨 𝘳𝘦𝘭𝘦𝘢𝘴𝘦 𝘵𝘩𝘢𝘵 𝘮𝘢𝘬𝘦𝘴 𝘮𝘶𝘭𝘵𝘪𝘱𝘭𝘦 𝘪𝘯𝘧𝘭𝘢𝘮𝘮𝘢𝘵𝘰𝘳𝘺 𝘤𝘭𝘢𝘪𝘮𝘴, 𝘪𝘯𝘢𝘤𝘤𝘶𝘳𝘢𝘵𝘦 𝘢𝘴𝘴𝘦𝘳𝘵𝘪𝘰𝘯𝘴, 𝘢𝘯𝘥 𝘧𝘢𝘭𝘴𝘦 𝘴𝘮𝘦𝘢𝘳𝘴 𝘵𝘰 𝘴𝘤𝘢𝘳𝘦 𝘵𝘩𝘦 𝘱𝘶𝘣𝘭𝘪𝘤 𝘪𝘯𝘵𝘰 𝘣𝘦𝘭𝘪𝘦𝘷𝘪𝘯𝘨 𝘵𝘩𝘢𝘵 𝘊𝘙𝘕𝘈𝘴 𝘸𝘪𝘭𝘭 𝘱𝘶𝘵 𝘰𝘶𝘳 𝘷𝘦𝘵𝘦𝘳𝘢𝘯𝘴’ 𝘩𝘦𝘢𝘭𝘵𝘩 𝘢𝘵 𝘳𝘪𝘴𝘬. 𝘉𝘶𝘵 𝘭𝘰𝘰𝘬 𝘤𝘭𝘰𝘴𝘦𝘭𝘺, 𝘢𝘯𝘥 𝘺𝘰𝘶’𝘭𝘭 𝘯𝘰𝘵𝘪𝘤𝘦 𝘵𝘩𝘦𝘴𝘦 𝘰𝘷𝘦𝘳-𝘵𝘩𝘦-𝘵𝘰𝘱 𝘤𝘭𝘢𝘪𝘮𝘴 𝘢𝘳𝘦 𝘮𝘪𝘴𝘴𝘪𝘯𝘨 𝘴𝘰𝘮𝘦𝘵𝘩𝘪𝘯𝘨 𝘪𝘮𝘱𝘰𝘳𝘵𝘢𝘯𝘵: 𝘢𝘯𝘺 𝘤𝘳𝘦𝘥𝘪𝘣𝘭𝘦 𝘦𝘷𝘪𝘥𝘦𝘯𝘤𝘦 𝘵𝘰 𝘣𝘢𝘤𝘬 𝘵𝘩𝘦𝘮 𝘶𝘱. 𝘖𝘯𝘤𝘦 𝘢𝘨𝘢𝘪𝘯, 𝘸𝘦 𝘢𝘴𝘬 𝘺𝘰𝘶 𝘵𝘰 𝘤𝘰𝘯𝘴𝘪𝘥𝘦𝘳 𝘧𝘢𝘤𝘵𝘴 𝘰𝘷𝘦𝘳 𝘵𝘩𝘪𝘴 𝘣𝘢𝘴𝘦𝘭𝘦𝘴𝘴 “𝘣𝘦𝘤𝘢𝘶𝘴𝘦 𝘐 𝘴𝘢𝘺 𝘴𝘰” 𝘢𝘳𝘨𝘶𝘮𝘦𝘯𝘵. 𝘈𝘴 𝘷𝘦𝘵𝘦𝘳𝘢𝘯𝘴 𝘸𝘩𝘰 𝘤𝘢𝘳𝘦 𝘢 𝘨𝘳𝘦𝘢𝘵 𝘥𝘦𝘢𝘭 𝘢𝘣𝘰𝘶𝘵 𝘰𝘶𝘳 𝘧𝘦𝘭𝘭𝘰𝘸 𝘣𝘳𝘰𝘵𝘩𝘦𝘳𝘴 𝘢𝘯𝘥 𝘴𝘪𝘴𝘵𝘦𝘳𝘴 𝘸𝘩𝘰 𝘩𝘢𝘷𝘦 𝘴𝘦𝘳𝘷𝘦𝘥 𝘵𝘩𝘪𝘴 𝘤𝘰𝘶𝘯𝘵𝘳𝘺, 𝘸𝘦 𝘧𝘦𝘦𝘭 𝘢 𝘳𝘦𝘴𝘱𝘰𝘯𝘴𝘪𝘣𝘪𝘭𝘪𝘵𝘺, 𝘵𝘰 𝘵𝘦𝘭𝘭 𝘵𝘩𝘦
𝘵𝘳𝘶𝘵𝘩 𝘢𝘯𝘥 𝘵𝘰 𝘴𝘦𝘵 𝘵𝘩𝘦 𝘳𝘦𝘤𝘰𝘳𝘥 𝘴𝘵𝘳𝘢𝘪𝘨𝘩𝘵.
𝘓𝘦𝘵’𝘴 𝘸𝘢𝘭𝘬 𝘵𝘩𝘳𝘰𝘶𝘨𝘩 𝘵𝘩𝘦 𝘮𝘰𝘴𝘵 𝘳𝘦𝘤𝘦𝘯𝘵 𝘴𝘵𝘢𝘵𝘦𝘮𝘦𝘯𝘵 𝘧𝘳𝘰𝘮 𝘵𝘩𝘦 𝘈𝘚𝘈 𝘤𝘭𝘢𝘪𝘮 𝘣𝘺 𝘤𝘭𝘢𝘪𝘮, 𝘵𝘰
𝘴𝘩𝘰𝘸 𝘫𝘶𝘴𝘵 𝘩𝘰𝘸 𝘸𝘦𝘢𝘬 𝘢𝘯𝘥 𝘧𝘢𝘶𝘭𝘵𝘺 𝘵𝘩𝘦𝘴𝘦 𝘵𝘪𝘳𝘦𝘥 𝘤𝘭𝘢𝘪𝘮𝘴 𝘢𝘳𝘦:
Members of Congress Call for CRNA Full Practice Authority Approval In VA
October 31, 2022
According to the letter, a national review of staffing shortages at the Veterans Health Administration (VHA) for fiscal year 2021 found anesthesiology shortages at numerous VHA facilities, including in Massachusetts, Rhode Island, New York, Pennsylvania, North Carolina, Florida, Tennessee, Michigan, Indiana, Illinois, Louisiana, Arkansas, Colorado, Oklahoma, Washington State, California, and Minnesota. "These anesthesiology workforce shortages have real consequences for our veterans, limiting access to high-quality care at a time when demand is growing for surgical procedures due to an aging veteran population," it stated.
New ParagraphCannabis Users May Feel More Pain Post Surgery
People who used marijuana reported worse pain and used more opioids after surgery compared with nonusers.
October 24, 2022
“Cannabis is the most commonly used illicit drug in the United States and increasingly used as an alternative treatment for chronic pain, but there is limited data that shows how it affects patient outcomes after surgery,” said lead author Elyad Ekrami, MD, clinical research fellow of the outcomes research department at Cleveland Clinic’s Anesthesiology Institute, in a press release.
It’s estimated that about 2.1 million Americans use medical cannabis, with 62 percent using it to treat chronic pain, according to U.S. Pharmacist.
“Our study shows that adults who use cannabis are having more — not less — post-operative pain. Consequently, they have higher opioid consumption after surgery,” says Dr. Ekrami.
The importance of removing barriers to care for Certified Registered Nurse [Anesthesiologist]
October 24, 2022
"CRNAs, as advanced practice registered nurses, are members of one of the most trusted professions, according to Gallup. Their expertise in anesthesia delivery, airway management and care of critically ill patients have made them highly sought-after healthcare providers during the COVID-19 pandemic and beyond.
"CRNAs play an important role in maintaining critical access in communities across the country," said Angela Mund, DNP, CRNA, president of the American Association of Nurse Anesthesiology (AANA). "They're often the only anesthesia providers in most rural hospitals and the predominant providers in underserved communities."
Despite their importance, CRNAs are hampered by current restrictions that require physician supervision of CRNAs. This federal requirement creates a barrier to expanding care and exacerbates the current provider shortage, especially in underserved communities."
"For more than two years, we have seen practice barriers removed at the federal level, allowing nurses to step up on the front lines of multiple global health challenges," said Mund. "We have seen how much nurses can do when we allow them to reach the full potential of their education and scope of practice."
Cannabis Users May Feel More Pain Post Surgery
October 24,2022
“Cannabis is the most commonly used illicit drug in the United States and increasingly used as an alternative treatment for chronic pain, but there is limited data that shows how it affects patient outcomes after surgery,” said lead author Elyad Ekrami, MD, clinical research fellow of the outcomes research department at Cleveland Clinic’s Anesthesiology Institute, in a press release.
It’s estimated that about 2.1 million Americans use medical cannabis, with 62 percent using it to treat chronic pain, according to U.S. Pharmacist.
“Our study shows that adults who use cannabis are having more — not less — post-operative pain. Consequently, they have higher opioid consumption after surgery,” says Dr. Ekrami.
Toxic Workplaces Could Damage Mental Health, Surgeon General Warns
October 20th, 2022
Long hours and cutthroat work conditions are harmful to workers’ mental and physical health, Surgeon General Vivek Murthy warned in a groundbreaking report on Thursday, the first time the surgeon general’s office has weighed in on potentially destructive effects of a toxic workplace as Americans reconsider their positions in mass numbers amid the so-called great resignation and phenomenon of quiet quitting.
Kentucky Adopts Favorable ASC rules
October 18, 2022
The Kentucky Cabinet for Health and Family Services has adopted amendments to the ambulatory surgery center (ASC) rules that remove the requirement for CRNAs to administer anesthetics “under the direction of the operating surgeon.” Kentucky has been an opt out state since 2012, and this revision aligns the ASC rules with Kentucky’s nursing law and hospital licensing rules. Comments in support of removing “direction” for CRNAs were submitted by the AANA, the Kentucky Association of Nurse Anesthetists, the Kentucky Nurses Association, and the Kentucky Hospital Association
AANA President Appointed to VA Committee on Rural Veterans' Health
October 5, 2022
Dr. Angela R. Mund, DNP, CRNA, president of the American Association of Nurse Anesthesiology (AANA), has been appointed to the Department of Veterans Affairs (VA) Veterans Rural Health Advisory Committee by the Secretary of the VA, Denis McDonough.
Certified Registered Nurse Anesthetists (CRNAs) are the primary providers of anesthesia in the U.S. military and serve in VA facilities across the country. They play a critical role in the VA healthcare system, ensuring veterans receive safe, cost-effective, and high-quality anesthesia care. Additionally, CRNAs are the primary provider of anesthesia in rural America.
ICAN Act Increases Patient Access to High Quality Healthcare
September 27, 2022
The Improving Care and Access to Nurses (ICAN) Act (HR 8812) recently introduced by Representatives Lucille Roybal-Allard (D-CA) and David Joyce (R-OH) will help ensure access to healthcare for millions of Americans by removing costly and unnecessary barriers to high-quality healthcare services. The American Association of Nurse Anesthesiology (AANA) supports this legislation, which will remove physician supervision of Certified Registered Nurse Anesthetists (CRNAs) and provide access to CRNA services in Medicaid.
"AANA thanks all the sponsors for introducing the Improving Care and Access to Nurses legislation," said AANA President Angela Mund, DNP, CRNA. "As the only anesthesia providers in most rural hospitals, and the predominant providers in underserved communities, CRNAs play an important role in maintaining critical access in communities across the country. However, superfluous regulations serve as barriers to expanding care, especially at a time when those same communities face a shortage of providers. This critical legislation will help ensure that everyone who needs access to the high-quality care provided by advanced practice registered nurses such as CRNAs can have it."
Ophthalmologists may be able to safely cut back on having anesthesiologists during cataract surgery
October 3, 2022
"Some type of anesthetic and possibly sedation is needed for cataract surgery, Chen noted, but the question is who should be present for administration and intraoperative monitoring of these patients. In the past, cataract surgery carried a much higher risk of complications, which helps explain the historic and legacy use of anesthesiologists and/or certified registered nurse anesthetists (CRNA)."
"The risk of the procedure itself used to require general anesthesia with paralysis and inpatient admission. Over time, ophthalmologists improved their technique so it [cataract surgery] is much safer and can be done on an outpatient basis," said Chen. "Often the patient just needs a topical anesthetic such as numbing drops in the eyeball, and, at UCSF anyway, a little fentanyl and midazolam, which are agents a sedation nurse can administer safely."
The question is: who's going to treat the bradycardia or astystole?
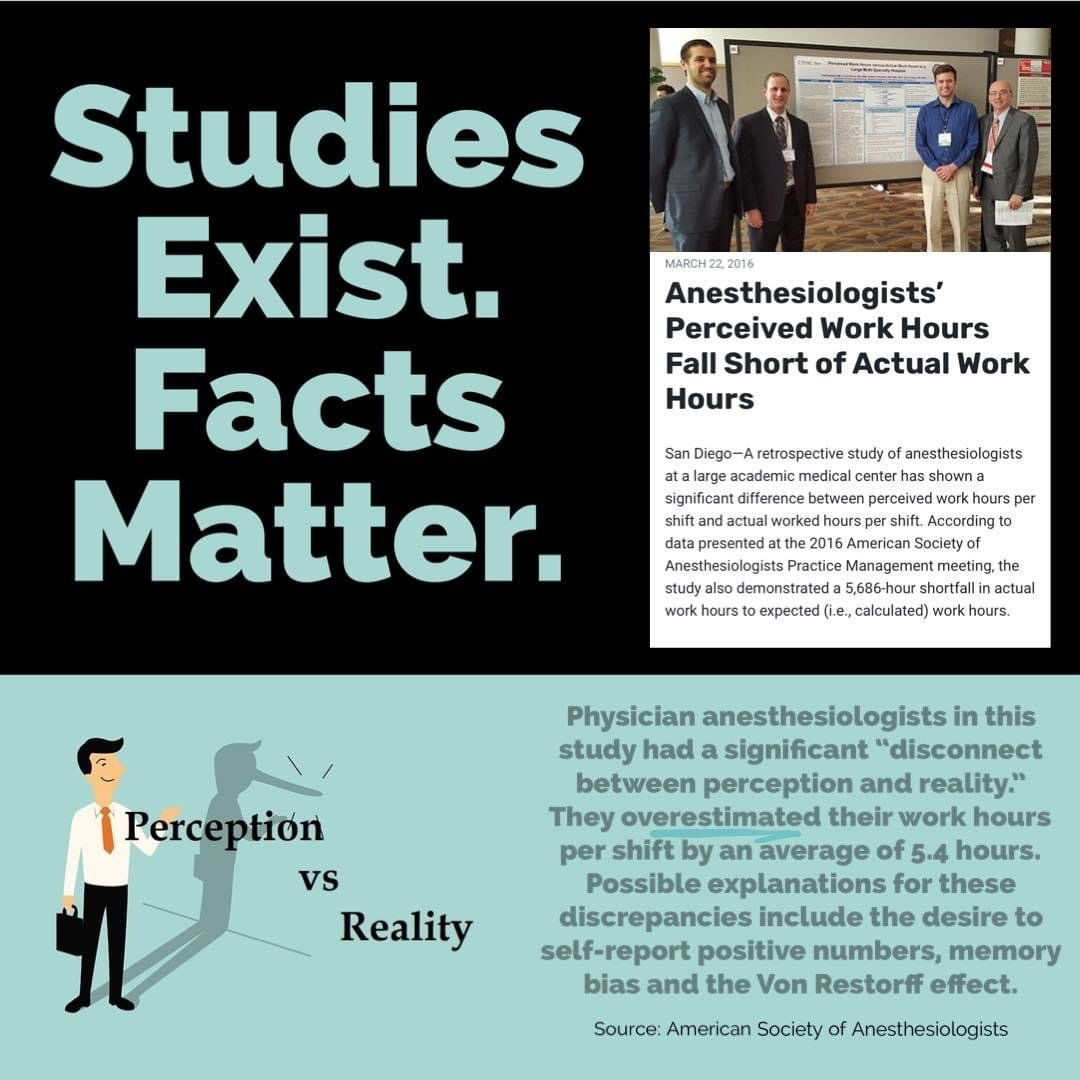
Physician Anesthesiologists
Suffer Significant Disconnect Between Reality and Perception
Presented at the American Society of Anesthesiologists in 2016